Female pattern baldness rarely looks dramatic at first. It often starts quietly with a widening part, reduced volume at the crown, or hair that no longer grows back the way it used to. Many women mistake it for stress or seasonal shedding and lose valuable time.
This guide explains female pattern baldness in practical terms. What causes it, how to slow it early, and which treatments actually help. We focus on prevention, medical options, daily care, and realistic expectations, so you can protect your hair with clarity instead of guesswork.
At a Glance: Female Pattern Baldness
Female pattern baldness isn’t a loss of identity. It’s a signal from your follicles that they need support. Hearing that signal early makes all the difference.
Timing shapes the outcome. When thinning is addressed early, follicles still have the strength to respond. Waiting too long limits what even the best treatments can do.
Consistency matters more than intensity. Using minoxidil regularly does far more than applying it perfectly for a few weeks and then stopping. Gaps slow progress.
Progress should be visible, not guessed. Monthly photos and checks using the Ludwig scale help separate real improvement from day-to-day worry.
Combination care works best. Minoxidil, anti-androgen support, PRP, and proper nutrition each support a different part of the hair cycle. Together, they create balance.
Timelines vary, and comparison rarely helps. Some women notice change within three months, others closer to nine. Hair grows slowly, but when it responds, it tends to keep going.
What Is Female Pattern Baldness (FPHL)?
Here’s the part no one tells you: female pattern baldness doesn’t mean you’re “going bald”. It means your hair follicles are gradually shrinking, quietly, invisibly, producing finer, shorter strands until the overall density thins. The medical name is female pattern hair loss (FPHL), and it’s the most common type of chronic hair loss in women.

Think of it like your hair volume is being turned down, not switched off. You still have the same number of follicles, they’re just producing weaker, smaller hairs that don’t cover the scalp as well as before.
According to the American Academy of Dermatology, nearly 40% of women over 40 experience FPHL, but many start noticing the first subtle signs, a wider part or a smaller ponytail, as early as their 20s and 30s. The condition usually follows a pattern: thinning at the crown and mid-scalp, while the frontal hairline often remains intact.
What’s happening biologically? It’s a mix of genetics, hormonal sensitivity to DHT (dihydrotestosterone), and sometimes life stage changes like menopause or PCOS. Over time, DHT shortens the hair’s growth phase (anagen) and extends the resting phase (telogen), leading to shorter, thinner hairs.
According to Cleveland Clinic, this process is non-scarring, meaning the follicles aren’t dead, just dormant. That’s why consistent treatment can reawaken them.
If you’ve ever looked at an old photo and thought, “Why does my part look wider now?”, that’s often the first visible sign. And yes, it’s treatable. The point is to start early, track progress, and stay consistent.
Early Signs You Can Spot at Home
The hardest part about female pattern baldness is that it creeps in quietly. No sudden clumps in the shower. No visible bald spot overnight. Just… a little less hair where there used to be more. Most women don’t even realize it’s happening until friends or hairstylists mention it.
Here’s a quick reality check: according to the American Academy of Dermatology (AAD), up to 40% of women over 40 experience some level of female pattern hair loss. Yet, most wait a year or two before doing anything about it. That waiting time matters. Once the follicles shrink beyond a certain point, they can’t bounce back.
The first subtle clues
- Your part looks wider than it did last year. Especially in photos or under harsh bathroom lighting.
- Your crown looks “see-through”. You might notice scalp glimmering under bright light or sunlight.
- Your ponytail feels thinner. Maybe it wraps around one more time than it used to.
- You see more scalp, not more strands. Shedding might be minimal, the problem is miniaturization, not fallout.
- Texture change. Hair feels finer, flatter, less bouncy, a classic FPHL sign.
Causes & Risk Factors of Female Pattern Baldness
Here’s the twist most people miss: female pattern baldness isn’t really about losing hair, it’s about how your follicles react to hormones and genes. The follicles are still alive; they’re just getting quieter.
Think of it like your Wi-Fi signal. The router (your follicles) still works, but the signal weakens over time. Sometimes it’s genetics. Sometimes hormones. Sometimes a mix that only a proper diagnosis can untangle.
Genetics: When It Runs in the Family
If your mother, aunt, or grandmother had thinning hair after 40, chances are your risk is higher. Research in the Journal of Investigative Dermatology shows that androgen receptor (AR) gene variations can make follicles more sensitive to DHT (dihydrotestosterone) , the hormone behind gradual miniaturization.
Dr. Mehmet Erdoğan ( Smile Hair Clinic ) explains,
“DHT shortens the hair’s growth phase. The result isn’t sudden baldness, but slow shrinking that reduces volume over years. Women often miss it until late.”
Hormones & Menopause
Estrogen usually protects hair follicles. But during perimenopause and menopause, estrogen levels drop while androgens stay steady — tipping the balance. That’s why many women first notice diffuse thinning at the crown around 45–55.
PCOS and Hormonal Imbalance
For younger women, polycystic ovary syndrome (PCOS) is a major trigger. Elevated androgen levels can lead to both acne and hair thinning at the top, ironic, but common. Dermatologists usually run blood tests for testosterone, DHEA-S, and thyroid function to pinpoint the pattern.
Stress, Nutrition & Medication
Chronic stress pushes more follicles into the resting (telogen) phase, which looks like diffuse shedding. Low ferritin (iron) or thyroid imbalance can make it worse. And yes, some birth-control pills or retinoids may trigger it too.
“Hair thinning in women isn’t always androgenetic. We rule out reversible causes first, it’s detective work, not guesswork,” says Dr. Güncel Öztürk from HairNeva Clinic.
The Bottom Line
Genes load the gun, hormones pull the trigger, and lifestyle keeps it firing. The good news? Each of these factors can be managed when caught early, often without surgical intervention.
How Doctors Confirm Female Pattern Baldness
You can’t fix what you don’t measure. That’s the quiet truth behind most failed hair-loss journeys. Many women buy serums, switch shampoos, and panic-scroll through forums, but skip the one step that gives real clarity: a professional diagnosis.
The visual pattern tells half the story
Dermatologists often spot female pattern baldness (FPHL) in seconds. The classic look? Thinner strands on the crown and along the central part, with the hairline mostly intact. They might use a tool called a dermatoscope, it magnifies the scalp to reveal miniaturized follicles that can’t be seen with the naked eye.
Dr. Güncel Öztürk explains,
“We look for a mix of thick and thin hairs in the same zone. That mosaic pattern is diagnostic. If the thinning is uniform or patchy instead, we think beyond FPHL.”
Tests that separate causes from copycats
Here’s what typically happens during evaluation:
- Detailed history: When thinning began, family history, menstrual cycle, medications, recent stress.
- Blood tests: Ferritin (iron storage), TSH and Free T4/T3 (thyroid), androgen profile if PCOS is suspected.
- Pull test: A few hairs are gently tugged to gauge shedding rate.
- Trichoscopy or dermoscopy: High-resolution scalp imaging for follicle diameter and density.
- Scalp biopsy (rare): Only if scarring alopecia or autoimmune loss is suspected.
Dr. Mehmet Erdoğan adds,
“We can’t treat what we don’t define. Many women actually have telogen effluvium from stress or nutrition, not true FPHL, mislabeling delays recovery.”
Why timing matters
Hair growth works on slow cycles, around 90 days per phase change. That means waiting six months “to see if it stops” can cost hundreds of follicles that might have been saved. Catching FPHL early allows doctors to preserve those semi-active roots before they switch off for good.
So if your scalp feels thinner, book a dermatologist visit before the next hair-care product haul. You might just save yourself a year of guessing.
Ludwig Scale: See Where You Are
Here’s the thing, that the most women with female pattern baldness (FPHL) underestimate how far it’s progressed. Not because they’re in denial, but because hair loss in women spreads diffusely, not in neat patches like it does in men.
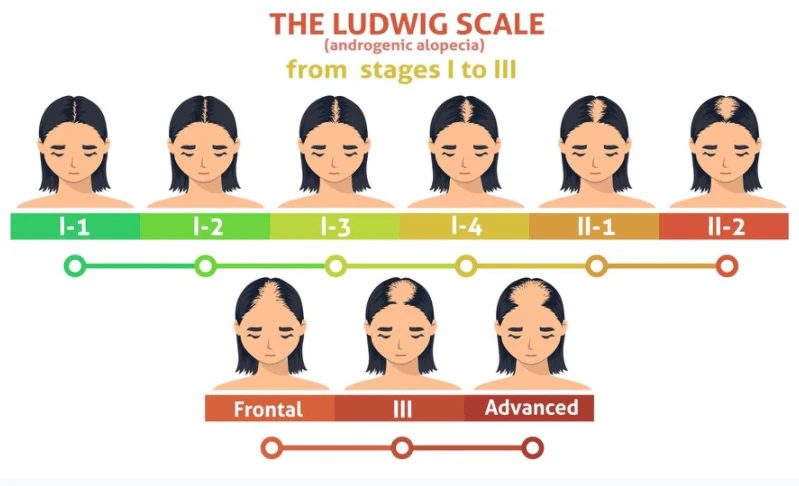
That’s why doctors rely on something called the Ludwig Scale. It’s a visual grading system that helps you (and your specialist) track what’s really happening on your scalp.
What the Ludwig Scale actually measures
Developed in the 1970s, it classifies female pattern hair loss into three main stages based on how much scalp is visible at the top of the head:
- Stage I: Slight thinning along the center part. The scalp might peek through under bright light, but coverage still looks decent.
- Stage II: The thinning widens into a noticeable strip, a clear “see-through zone” running from the front to the crown.
- Stage III: Diffuse thinning across the top with sparse density, sometimes leaving only a thin fringe of hair.
Dr. Güncel Öztürk puts it simply:
“Stage I patients often panic, while Stage III patients arrive too late. The right time to act is when you first see that light reflection along your part.”
Why this matters
The Ludwig Scale isn’t about labeling you; it’s about tracking. Think of it as your progress chart. Taking monthly photos in the same lighting lets you see micro-changes, the kind you’d never notice day to day. According to the American Academy of Dermatology, early treatment at Stage I can preserve up to 30 % more follicular density compared to delayed intervention.
So before you panic-Google “how bad is my hair loss”, grab your phone camera instead. One photo a month, same angle, same light, can give you more truth than any mirror.
Treatment Ladder: What to Start, What to Add, When to Refer
Here’s a small truth that surprises most women: female pattern baldness (FPHL) doesn’t have a “one magic fix.” It’s more like tuning an orchestra, you start with one instrument (usually topical minoxidil) and add others gradually until the rhythm feels right.
Step 1: Start with Minoxidil and stay consistent
Topical minoxidil remains the first-line treatment for female pattern hair loss, backed by decades of dermatology research. Available in 2% or 5% foam or solution, it helps by extending the growth phase (anagen) of hair follicles.

Here’s the catch: the first few weeks might bring increased shedding. Don’t panic, that’s your old hairs making room for thicker ones. Most women start noticing texture improvement by month 3–4 and visible density by month 6.
Dr. Mehmet Erdoğan says,
“Think of minoxidil like brushing your teeth. It only works when it’s routine. Miss a week, and follicles slip back to resting mode.”
If your scalp gets irritated, switch to foam (less alcohol) or use a ketoconazole shampoo twice weekly, it reduces inflammation and DHT buildup.
Step 2: Add Supportive Treatments (when needed)
If minoxidil alone doesn’t deliver, doctors may layer in:
- Low-dose oral minoxidil (LDOM): Usually 0.25–1 mg daily under supervision. Studies published in JAMA Dermatology 2023 show promising density gains with minimal side effects.
- Spironolactone: Works as an anti-androgen. Great for women with PCOS or hormonal imbalance.
- Finasteride/Dutasteride: Used off-label in postmenopausal women. Must avoid during childbearing years.
- PRP therapy: Concentrated platelets stimulate dormant follicles. Often done monthly for 3 sessions, then maintenance.
- Low-Level Laser Therapy (LLLT): At-home laser combs or helmets that improve circulation and cellular energy in follicles.
Dr. Güncel Öztürk notes,
“Combination therapy gives synergy. Minoxidil wakes follicles; PRP nourishes them; spironolactone stops new damage.”
Step 3: Know When to Refer
If there’s no improvement after 12 months of consistent use, or if your Ludwig Stage progresses, a hair transplant evaluation may help. Women with stable donor zones respond well to FUE or DHI techniques when medical management has slowed progression.
Dr. Güncel Öztürk advises,
“Surgery doesn’t replace medical therapy, it completes it. Patients who continue minoxidil after transplant see stronger graft survival and density.”
The practical rhythm
Start small. Track your scalp photos monthly. Adjust based on your dermatologist’s review every 3–4 months. The point isn’t speed, it’s steadiness.
So no, there’s no miracle serum. But there is a map. Follow it patiently, and your scalp might just surprise you.
Your 12-Week Starter Plan for Female Pattern Baldness
If you’re like most women who notice thinning, you want a plan, not vague encouragement. So here’s a realistic 12-week roadmap that blends medical science.
It’s simple, consistent, and meant to help you take back control.
Weeks 1–2: The Baseline Phase
Start documenting before you start treating.
- Take three photos of your scalp: front, crown, and part line, under the same natural light.
- Begin topical minoxidil 5 % once nightly on dry scalp. Massage it in gently for 30 seconds.
- Wash with ketoconazole shampoo twice a week to control DHT buildup and inflammation.
- Note any irritation or dryness. If it happens, switch to foam or reduce frequency to once every 2 days.
Weeks 3–6: The Adjustment Phase
This is when some women see mild shedding. It’s actually a sign that minoxidil is pushing old hairs out to start a new growth cycle.
- Stay consistent, missing days resets progress.
- Add biotin (2.5 mg) or iron supplements only if your doctor confirms low ferritin.
- If you have hormonal triggers like PCOS, ask about adding spironolactone (25–50 mg/day).
- Schedule your first follow-up visit at week 6 to evaluate tolerance and scalp condition.
Dr. Mehmet Erdoğan notes,
“Shedding freaks people out, but it’s pruning, not damage. You’re clearing the path for stronger regrowth.”
Weeks 7–10: The Activation Phase
You should start feeling tiny baby hairs sprouting along your part or temples. They’re soft and colorless at first, don’t dismiss them.
- Keep using minoxidil daily.
- Add PRP therapy if your dermatologist suggests it; two sessions during this phase often jump-start visible growth.
- Focus on scalp health: gentle brushing, no tight hairstyles, avoid harsh chemical treatments.
- Continue your monthly photo tracking.
Weeks 11–12: The Reflection Phase
By now, the biggest change isn’t just in your hair, it’s in how you feel. You’ve built a habit, gained data, and reduced that helplessness so many women describe.
- Compare your week-12 photos with week-1.
- Schedule your next evaluation for month 4 to discuss adjustments (like adding oral minoxidil 0.25 mg if density is still low).
- If you see no progress, it’s time for deeper bloodwork and possibly a trichoscopy scan.
Dr. Güncel Öztürk says,
“We tell patients: it’s not a sprint, it’s gardening. Tend it, water it, measure progress by seasons, not weeks.”
So, take a breath. You don’t have to fix everything overnight, just start the 12-week rhythm. That’s how recovery begins.
Who Might Consider a Hair Transplant
Here’s the honest truth most clinics won’t lead with: not every woman with female pattern baldness (FPHL) is a good candidate for a hair transplant. And that’s not bad news, it just means the approach has to match your hair biology, not someone else’s success story online.
When a transplant can make sense

Hair transplantation for women works best when the donor area (usually the back of the scalp) still has dense, stable follicles. These grafts are genetically resistant to DHT, so they keep growing even when transplanted to thinning zones.
Dr. Güncel Ötürk explains:
“Our best results come from patients whose loss has stabilized with medical therapy. Transplant fills visible gaps, but long-term density depends on continuing minoxidil or anti-androgen care afterward.”
A good candidate typically:
- Has Ludwig Stage I or II thinning with clear donor density.
- Has controlled hormonal or nutritional causes.
- Understands that grafts add coverage, not infinite volume.
- Is emotionally ready for a 6–12-month wait before full results.
When it might not be right (yet)
If your thinning is still spreading, or your donor area looks patchy, a transplant might worsen density balance. Same goes if you haven’t tried minoxidil, PRP, or spironolactone yet. Those treatments often “buy time” and stabilize shedding before any surgical step.
Dr. Mehmet Erdoğan notes:
“Women with diffuse FPHL often respond beautifully to combination therapy. Surgery comes only after the scalp environment is stable.”
Setting expectations — not filters
Transplanted hair doesn’t magically thicken the entire scalp. It’s strategic: creating optical density by redistributing follicles. Think of it like rearranging books on a shelf, you fill empty spots to make it look full, not to double the number of books.
Dr. Güncel Öztürk sums it up:
“Surgery should be your final polish, not your first step. Healthy donor management is everything.”
If you’re unsure, ask your doctor for a trichoscopy density report before jumping into surgery. It’s the closest thing to a roadmap for your scalp’s future.
Safety, Side Effects, and When to Pause Treatment
Every treatment that actually works carries some level of trade-off. That doesn’t mean you should fear it, it means you should understand it. The goal isn’t to avoid every side effect; it’s to know which ones are normal, which aren’t, and when to hit pause.
Minoxidil: The shedding that scares everyone
Let’s start with topical minoxidil, since it’s the cornerstone for female pattern baldness. The most common “side effect” isn’t actually harmful, it’s temporary shedding in the first 4–6 weeks. That happens because the follicles are shifting phases. Other short-term issues might include:
- Mild scalp irritation or dryness
- Unwanted fine facial hair (rare and reversible)
- Dandruff-like flaking if you use too much solution
Oral options: Small pills, big responsibility
Low-dose oral minoxidil and spironolactone can be powerful, but they require monitoring. Expect mild side effects like puffiness, light dizziness, or body hair growth at higher doses.
- Women on spironolactone should have potassium levels checked every few months.
- Oral minoxidil may slightly lower blood pressure, so if you already take BP meds, discuss dosage adjustments.
When to pause or switch
Stop and consult your dermatologist if you experience:
- Persistent scalp redness or sores
- Swelling in hands or feet
- Irregular periods or breast tenderness (spironolactone)
- Heart palpitations or shortness of breath (oral minoxidil, though rare)
Pregnancy, breastfeeding & hormonal shifts
Minoxidil, finasteride, and spironolactone aren’t safe during pregnancy or breastfeeding. If you’re planning to conceive, talk to your doctor early, they can help transition you off gradually.
The mindset that matters
Think of this as long-term skincare for your scalp. You’ll tweak doses, pause when needed, and resume smarter. A patient at our partner clinic once paused minoxidil during summer travel, lost progress by month 3, and regained it after restarting, proof that consistency beats perfection.
So yes, safety matters, but fear shouldn’t stop you from taking action. With proper supervision, the balance tilts strongly in your favor.
Tracking Progress the Smart Way
Most women say the same thing after starting treatment for female pattern baldness (FPHL) and “I can’t tell if it’s working”. That uncertainty can mess with your motivation faster than any side effect. But here’s the good news: progress is measurable. You just need a system that beats memory and lighting tricks.
The photo method that never lies
Forget filters. You need consistency.
- Take clear scalp photos once a month with the same light, same angle, same time of day.
- Use natural light near a window or consistent white LED lighting.
- Focus on your center part, crown, and temple edges.
After 12 weeks, line them up side-by-side. The changes are subtle, new baby hairs reflecting differently, less scalp glare, part line slightly narrower. That’s where the real proof lives.
Use simple tracking tools
- Trichoscopy or AI scalp scan: Clinics use these to measure follicle density per cm². Many now offer follow-ups every 3 months.
- Hair diary: A notebook or app where you note shedding patterns, texture changes, or new baby hairs.
- Ludwig Scale reference photos: Keep one handy to mark your current stage, it helps visualize progress in context.
Expectation check
Here’s the typical pattern if you stay consistent:
- Months 1–2: Initial shedding, maybe mild irritation.
- Months 3–4: Texture improves; scalp feels thicker to the touch.
- Months 5–6: Noticeable volume at the crown or part line.
- Months 9–12: Density stabilizes; baby hairs mature.
A quick myth to drop
Many believe “no visible regrowth” after three months means it’s not working. Not true. Hair grows in 90-day cycles, so visual change often lags behind follicle recovery. Give it at least six months before judging.
So treat your progress tracking like journaling, quiet, honest, and surprisingly empowering. You’ll know when things are changing, even before anyone else notices.
Common Questions & Answers on Female Pattern Baldness
What is Female pattern baldness (FPHL)?
Female pattern baldness (FPHL) is a gradual thinning of hair across the crown and part line caused by hormonal and genetic factors. Early treatment with minoxidil, PRP, or anti-androgen therapy can slow follicle miniaturization and restore density within 3–6 months. Diagnosis and consistency are key to lasting regrowth.
Can female pattern baldness be reversed?
Partially yes, especially if caught early. Treatments like topical or oral minoxidil, PRP, and anti-androgens can regrow miniaturized hairs and thicken existing ones. But once a follicle is completely inactive (fibrosed), it can’t regrow hair.
How long before I see results?
Expect the first visible changes between 3–6 months, with fuller results at 9–12 months. That’s how long it takes for follicles to complete one growth cycle. Early patience pays off, stopping too soon resets everything.
Are side effects common with minoxidil?
Most women tolerate topical minoxidil well. Mild dryness or irritation can happen early on. The “shedding phase” in the first few weeks isn’t dangerous, it’s part of the growth reset. Persistent redness or swelling? Time to talk to your dermatologist.
Can lifestyle alone stop hair loss?
Healthy habits help, but they can’t replace medical treatment. Protein-rich diet, iron levels above 50 ng/mL, stress management, and scalp hygiene make results stronger, but don’t stop follicle miniaturization on their own.
What’s the difference between female pattern baldness and telogen effluvium?
FPHL causes gradual thinning and widening of the part. Telogen effluvium causes sudden, diffuse shedding triggered by stress, illness, or childbirth. The latter usually recovers within 6 months; FPHL is chronic and needs treatment.
Can you regrow temple or frontal hairs?
Temples are the hardest zone, density here drops first and responds slowest. PRP and low-dose oral minoxidil have shown modest success, but most improvement happens at the mid-scalp and crown.
Will hair loss stop if I stop birth control?
Sometimes yes, especially if your pill contained androgenic progestins. But some women experience a rebound shed 2–3 months after stopping. Always discuss transitions with your doctor.
What if I stop using minoxidil after a year?
Regrown hairs will eventually miniaturize again within 3–6 months of stopping. FPHL is chronic; maintenance matters. If you need a break, reduce frequency gradually instead of quitting cold.
Does stress really cause permanent hair loss?
Stress-related shedding (telogen effluvium) is temporary. But chronic cortisol elevation can accelerate androgen sensitivity, making female pattern baldness progress faster. Think of stress as gasoline poured on a slow fire.
Is hair transplant safe for women with FPHL?
Yes, when performed on the right candidate with stable donor density. Most women with Stage I–II thinning benefit most. Transplants restore coverage; medications protect it long-term.
Which shampoo or routine is best for FPHL?
Use a mild ketoconazole shampoo twice weekly, alternate with a sulfate-free cleanser, and massage gently to improve circulation. Avoid tight hairstyles, high heat, and heavy silicones that clog follicles.
Can female pattern baldness happen in your 20s?
Yes. Rising PCOS rates and stress-related hormonal shifts mean more women under 30 are seeing early-onset FPHL. The earlier you start treatment, the better your long-term density retention.
Glossary of Terms
FPHL (Female Pattern Hair Loss)
The most common type of hair thinning in women, caused by gradual follicle miniaturization rather than sudden shedding.
DHT (Dihydrotestosterone)
A hormone derived from testosterone that can shrink hair follicles over time, leading to thinner, shorter strands.
Miniaturization
The process where hair follicles shrink and produce finer, weaker hairs — the hallmark of FPHL.
Anagen Phase
The active growth stage of the hair cycle, usually lasting 3–5 years. Treatments like minoxidil help extend this phase.
Telogen Phase
The resting stage when old hairs prepare to shed. In FPHL, too many follicles enter this phase early.
Ludwig Scale
A visual chart doctors use to classify the stages of female hair thinning from mild widening of the part (Stage I) to diffuse crown loss (Stage III).
Minoxidil
A topical or oral medication that stimulates follicles to produce thicker hair. It’s the first-line treatment for FPHL.
PRP (Platelet-Rich Plasma)
A procedure where your own platelets are injected into the scalp to boost growth and healing.
Spironolactone
A medication that blocks androgens (male hormones) that can worsen hair thinning in women.
Trichoscopy
A magnified scalp imaging test that helps measure follicle health, density, and progress over time.
Low-Level Laser Therapy (LLLT)
A non-invasive light-based treatment that improves scalp circulation and supports hair regrowth.
Telogen Effluvium
A temporary shedding condition often triggered by stress, illness, or hormonal changes — not the same as FPHL.